What is a Urinary Tract Infection (UTI)?
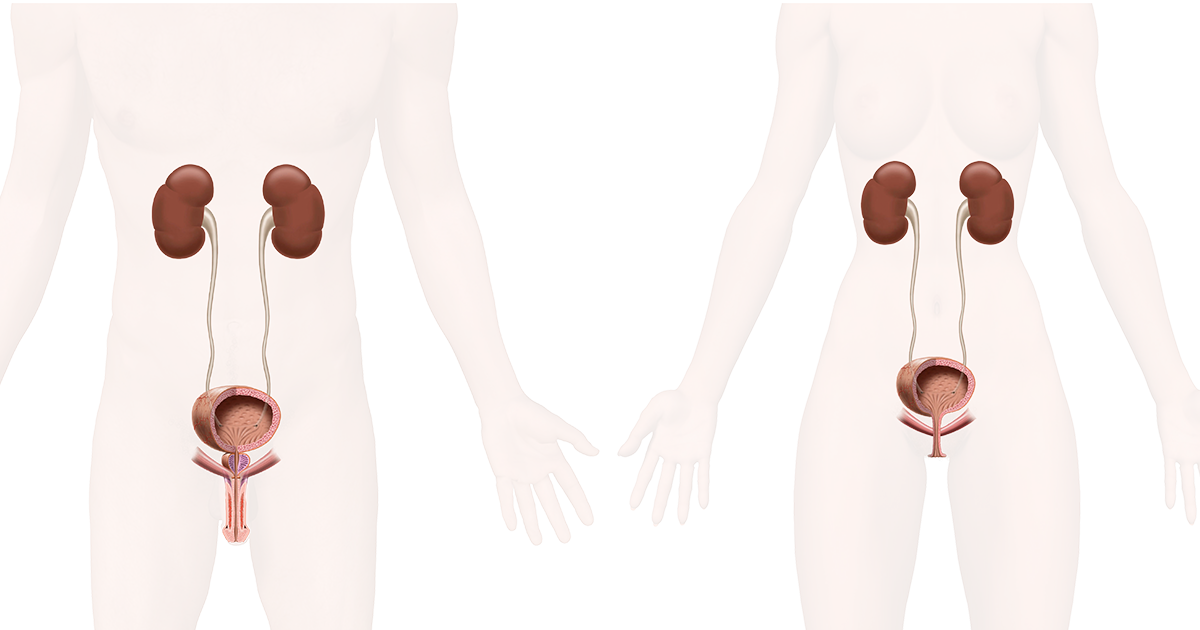
A urinary tract infection (UTI) can affect any part of the urinary system and is caused by bacteria. Most commonly, the infection involves the lower urinary tract, which is the bladder and the urethra. Almost 90% of UTIs are caused by the bacteria 'Escherichia coli (E. coli)' and this bacterium is often present in our gut without causing any harm.
Women are at greater risk of developing a UTI than men, for several reasons. Infections limited to the lower urinary tract can be very painful and troubling but normally go away on their own after a few days. If not, treatment with antibiotics might be required. However, if the UTI is not defeated and bacteria spreads to the kidneys, the consequences may be serious. In all cases a UTI can be very troublesome – but there are steps to take to reduce the risks of getting a UTI.
What are the Typical Symptoms of a Urinary Tract Infection (UTI)?
Urinary tract infections typically cause one or more of the following symptoms:
- Pain or a burning feeling whilst urinating
- Frequent urination (often small volumes)
- Urine that appears cloudy or smelly
- Urine with signs of blood or red color
- Pressure or cramping in the lower abdomen (in women especially in the center of the pelvic area)
Depending on which part of the urinary system is infected by bacteria, the signs and symptoms differ.
Typical Kidney Infection Symptoms are:
- High fever
- Chills or shaking
- Lower back pain or pain in the side of your back
- Nausea or vomiting
UTIs are an issue of concern for many reasons and therefore you should always seek medical advice if you experience troublesome symptoms.
What Causes a Urinary Tract Infection (UTI)?
A urinary tract infection typically occurs if bacteria travels along the urethra into the bladder, begins to multiply and causes tissue damage. The human body has defense mechanisms to protect against these invaders, but these defenses sometimes fail. The immune system varies between individuals, therefore the level of defense mechanisms differs. If the bacteria win the battle over the body’s immune system, we will react with symptoms, e.g. pain and fever.
Watch this 3-minute animation to understand how a UTI occurs:
Who is More at Risk of Getting a Urinary Tract Infection (UTI)?
Urinary tract infections are more common in women than in men because of a number of reasons. The shorter urethra makes it easier for bacteria to travel along the urethra and infect the bladder, and the short distance between the anus and the urethral opening can increase the risk of contamination as E.Coli are normally present in the gut and may migrate and lead to an infection.
Other risk factors for contracting a UTI include catheter use and bowel problems such as constipation.
Why are Women at Higher Risk of Getting UTIs Than Men:
- Female anatomy, as the shorter urethra makes it easier for bacteria to reach the bladder.
- Sexual intercourse, because of potential transfer of bacteria (vagina close to rectum).
- Changes in vaginal flora, e.g. via the use of spermicides.
- Pregnancy due to hormonal changes etc.
- Menopause, with declining levels of estrogen.
General risk factors for UTIs, related to both men and women:
- Structural problems in the urinary tract e.g. abnormalities of the urinary tract from birth or enlarged prostate (in older men)
- A low immune system or when the body is coping with 2 or more diseases together
- Bowel dysfunction (constipation makes it more difficult to empty the bladder)
- Catheter use (anything inserted into the urethra, including surgical examinations performed at hospitals, actually increase the risk of infection)
How are Urinary Tract Infections Treated?
Normally a UTI will go away by itself after a few days if there are no other underlying diseases. However, there are people who will need antibiotics to combat the infection. People who get frequent UTIs usually require specific treatment and for a severe UTI and/or effect on the kidneys, intravenous antibiotics in a hospital may be needed. If a UTI is suspected, referral to a healthcare professional should always be done.
How can Urinary Tract Infections be Prevented?
There are things you can do to reduce the risks of getting a UTI.
Prophylactic (preventative) treatments, like drinking cranberry juice making the urine more acidic were initially thought to contribute to an antibacterial effect, but there is no solid scientific proof that this works. The most important factor in UTI prevention is to inhibit the bacteria from attaching to the cell wall of the bladder. Cranberries contain a substance that has been shown in studies to be able to hinder the bacteria from attaching. It is however only the whole cranberry fruit that shows this effect, not the juice. Also, a combination of cranberry and propolis (a substance from plants used in food) has shown indications of prophylactic action, as propolis hinders the bacteria from attaching to the bladder wall.
People with healthy and variable normal bacterial flora are shown to have the strongest defense mechanism against urinary tract infections. By adding probiotics (living microorganisms) the normal flora may grow and some studies suggest this is an attractive strategy to prevent infection.
- Probiotics: means live bacteria found in certain foods or supplements. They can provide numerous health benefits.
- Prebiotics: These substances come from types of carbs (mostly fiber) that humans can’t digest. The beneficial bacteria in your gut eat this fiber.
Additional Things Known to Help Prevent UTIs:
Drink plenty of liquids: Drinking water helps dilute the urine and ensures that urination is done more frequently, allowing bacteria to be flushed away from the urinary tract and bladder before an infection can begin.
Wipe from front to back to avoid the transfer of bacteria from the rectum to the urethra (in females). Urinating directly after having sex helps flush bacteria away from the urethra and bladder.
Avoid constipation, studies show that this may cause the bladder to not empty completely, leaving residual urine containing bacteria.
What is the Urinary Microbiota and How Does This Link to Urinary Tract Infection (UTI)?
Urine is no longer believed to be sterile, and it’s known that a large number of bacteria coexist (live together) in the urinary tract, without causing symptoms. The bacteria create a symbiotic relationship (benefit to each other), and this protects against infection from more harmful strains. The term urinary microbiota refers to a variety of bacteria present in healthy people without any signs or symptoms of infection. This area gained focus along with the development of new more advanced and sensitive methods to actually find and identify bacteria. The number and variety of bacteria living in symbiosis with us in the urinary tract are believed to play a role in the development of many diseases, including UTIs. This is a rather new area, gaining a lot of attention in current research.
Sometimes used interchangeably, these two terms have subtle differences:
- Microbiota can refer to all the microorganisms found in an environment, including bacteria, viruses, and fungi.
- Microbiomes are individual to each organism; the diversity in microbiomes between individuals is huge.
Why are Urinary Tract Infections (UTIs) an Area of so Much Concern?
UTIs are complex, in some patients they may go away spontaneously, whilst in others they may cause severe consequences. UTIs are the most common bacterial human infection and it’s estimated that UTIs affect more than 130 million people globally each year. Many of these patients are treated with antibiotics, contributing to the rapidly increasing antimicrobial resistance.
Antimicrobial resistance occurs when bacteria change over time and no longer respond to medicines. This makes the infections harder to treat, increases the risk of disease spread, and prolongs the time before patients recover. According to WHO, the problem of antimicrobial resistance is so serious that it threatens our modern healthcare system. By 2050 it may cause 10 million deaths or more if we lose our ability to use effective antibiotics. The alarming threat of antimicrobial resistance needs to be taken seriously and be fought at different levels.
What are Risk Factors for Urinary Tract Infection (UTI) in Conjunction to Catheter Users?
Individuals who cannot empty their bladder in a natural way are dependent on catheterization. Intermittent catheterization (IC) is the gold standard and should always be chosen over indwelling catheters to prevent infections. IC means that a small plastic tube is inserted into the urethra and discarded after use. The procedure mimics the body´s natural way of emptying and nothing remains in the body longer than the time needed to completely empty the bladder. This is of major importance to avoid infections. Indwelling catheters remain in the body for weeks or months and having something in place inside the body helps bacteria attach and travel along this surface to the bladder resulting in an infection. Individuals using indwelling catheters often get UTIs that are much harder to treat with regular antibiotics. This is due to more aggressive types of bacteria as well as different bacteria species present at the same time.
IC is the best way of emptying the bladder, for those who cannot urinate naturally. However, there is a risk of UTI and special attention needs to be taken to avoid this risk as much as possible. The increased risk of UTIs is because of several reasons:
- Risk of inserting foreign bacteria via the catheter
- Loss of natural flushing of the urethra while using a catheter (compared to natural voiding)
- Risk of the catheterization procedure making wounds in the urethra
- Remaining urine in the bladder due to incomplete emptying of the bladder, leaving residual urine containing bacteria
For people who need help to empty their bladders fully, intermittent catheterization provides many advantages, e.g. it will empty the bladder completely, it can be done independently and it’s quick and easy once you are familiar with the therapy. In addition, it maintains normal bladder function in a way that is not the case for indwelling catheters. However, despite all the advantages, there is an increased risk for UTIs compared to normal urination. In fact, everything inserted into the urethra will potentially increase the risk of UTIs, therefore this is a topic of extra concern for these individuals. Important to know is that not all intermittent catheters are the same. By selecting a catheter with specific catheter requirements, the risk of UTIs can be minimized.
Watch this 2-minute animation to know how the risk for UTIs can be reduced:
Not All Catheters Are the Same
Different types of intermittent catheters are available to suit individual needs and it’s important to remember that there are still differences among the hydrophilic catheters available on the market. One important part is the lubricated surface (catheter coating) that will be in contact with the urethra. Usually, catheterization is performed 4-6 times a day, or over 1800 times per year, hence it’s crucial to select a catheter with optimal coating to avoid causing friction, wounds, discomfort and UTIs in the long run. The catheter coating needs to stay lubricated during both insertion and withdrawal (after the bladder has been emptied). This is to ensure that no harm is caused to the sensitive urethra.
A poor surface could not only cause pain but also cause irritation or trauma to the urethra - and a damaged tissue is more prone to attract bacteria and cause a UTI.
LoFric is the world’s first hydrophilic catheter, invented already in 1983. With the longest time available on the market, Wellspect has comprehensive clinical evidence available of LoFric’s unique coating which stays lubricated during the whole catheterization procedure. Data shows that LoFric catheters reduce the risk for UTIs with 64%* because of the unique surface coating which protects the urethra from harm, and thereby limits the risks for infection. This is of utmost importance for individuals in need of catheterization, both short- and long-term.
*Li et al., Arch Phys Med Rehabil., 2013 - compared to non-hydrophilic catheters

Key Take Home Message
UTIs are an issue of concern since they are troublesome and may lead to serious consequences if not treated. Catheter users are at higher risk of UTIs compared to people emptying their bladders in a natural way. Intermittent catheterization should always be selected over indwelling to prevent infections. There are differences between intermittent catheters and these are very important to be aware of to reduce the risk of obtaining UTIs. LoFric has a unique surface shown in several clinical studies to be superior in terms of reducing friction, and wounds to the urethra and reducing the risk of UTIs.
When Selecting the Type of Intermittent Catheter:
- Select a catheter with a surface coating that remains lubricated during the whole catheterization procedure (wounds in the urethra will make it easier for bacteria to cause a UTI).
- Select a catheter that will empty the bladder completely to avoid residual urine (bacteria that remain in the bladder increase the risk of a UTI).
- Use an insertion grip to avoid touching the catheter surface with the hands while inserting the catheter (foreign bacteria increase the risk of developing a UTI)
To learn more about our LoFric catheters and to order free product samples, please press the button below: