Fecal incontinence (FI) is the symptom that is ranked as the most bothersome for patients. FI is also the most under reported due to the taboo nature and embarrassment associated with it.
There are different reports of prevalence with variations from 0.4 to 18% of the population. A higher prevalence is sometimes reported in females and commonly seen in the elderly, which may be due to the anatomical differences in gender, and thereafter due to factors associated with the aging process.
Definition and classifications
The definition of FI is the involuntary loss of rectal contents (feces) through the anal canal and the inability to postpone an evacuation until socially convenient.
There are 3 classifications of FI symptoms;
- passive incontinence: defined as involuntary loss of feces without the feeling of urgency or need to defecate,
- urge incontinence: defined as loss of bowel contents despite attempts to retain contents,
- mixed incontinence: defined as both passive and urge symptoms.
Assessment, diagnosis, and treatment of FI need to be tailored for each individual person.
Treating FI
Fluid and diet
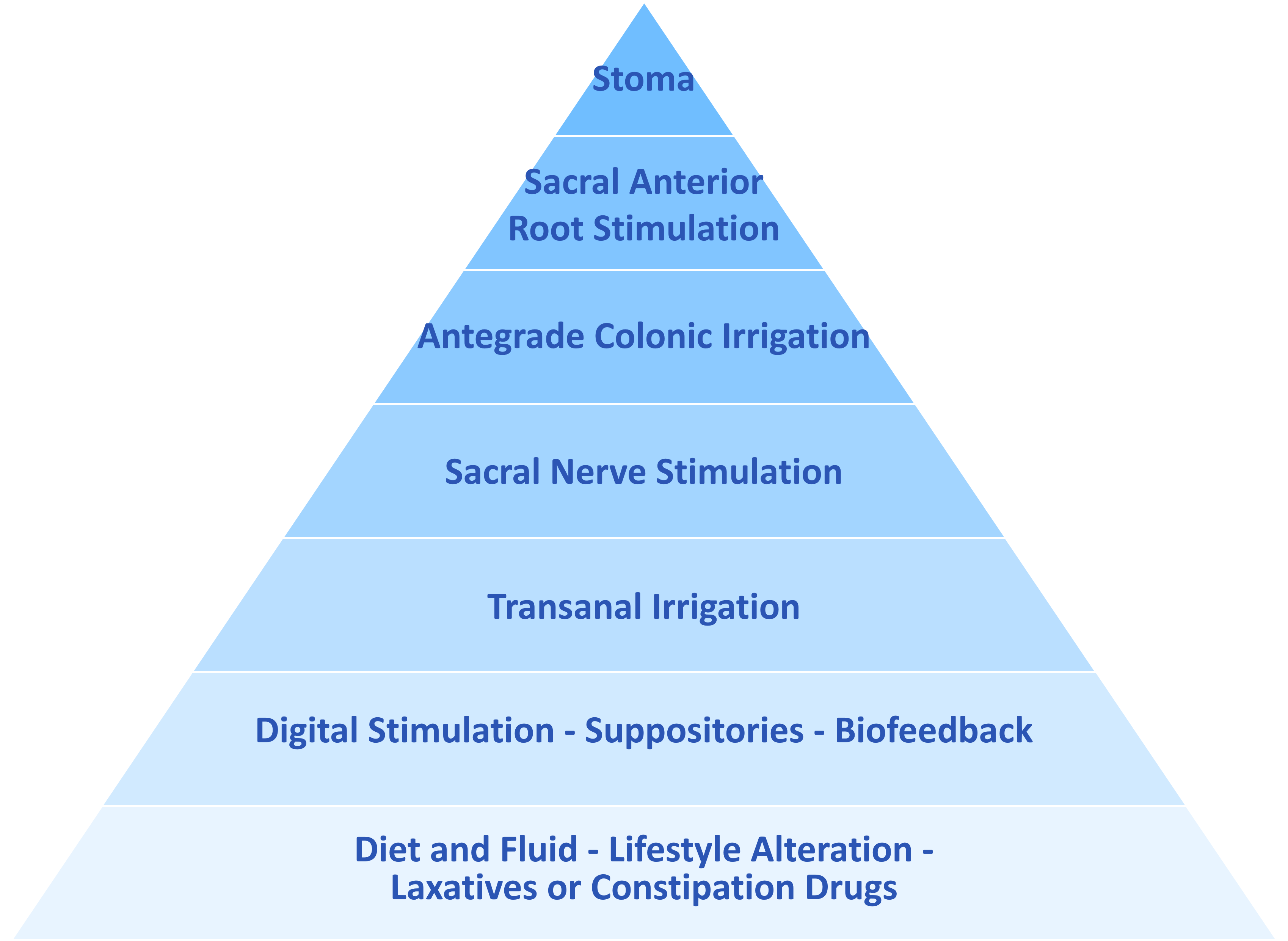
Standard bowel care with lifestyle changes and drugs are the first treatment steps. To achieve an effective treatment, adherence not only to drugs but also to lifestyle changes requires understanding and acceptance of the therapy.
Thereafter treatments should be offered in line with the bowel management pyramid:
Pharmacological treatments
Pharmacological treatments, including oral preparations and suppositories, have shown low response rates, 20-40%, in randomized clinical trials with symptom-based primary end-points.
Transanal irrigation
Transanal irrigation is a good treatment for some as the management of fecal incontinence and has shown to improve symptoms of FI as well as of quality of life, and socialization, and it avoids the need for escalation of more invasive treatments.
Read more about Transanal Irrigation (TAI).
Sacral Nerve Stimulation and surgical treatment
Neuromodulation such as sacral nerve stimulation (SNS) has been reported to reduce symptoms by 50% for FI in about 67 to 100% of the patients in clinical studies. This treatment may not be offered in all geographical areas. Where this treatment is not provided, or not suitable, individuals may be assessed by specialist surgeons for consideration of a stoma to manage their symptoms.
Additional coping strategies
The goal of bowel management is to reduce the number of FI episodes and improve quality of life. Despite the variety of treatment options, many people do not achieve a significant and long-term improvement in the reduction of episodes. This means that many patients may still need to use containment products, fecal inserts, and barrier creams to cope with their symptoms. Incontinence pads/nappies only serve to contain any feces from leaking onto clothes or bed linen/equipment etc.
There is no device available that could remove feces away from harming the outer skin after leakage, so for anybody who has lost control of their bowels – the containment pad must be changed immediately, and the skin cleansed.
A fecal insert is a passive barrier to help prevent FI episodes that provides immediate results and could be a stand-alone therapy or be used in conjunction with other treatments such as biofeedback, dietary modifications, and/or the use of medications. The difference between fecal inserts and incontinence pads is that inserts are more invasive, but have the advantages of better odor control and reduced potential skin problems. It may be that barrier cream may also be needed to stop further damage to the delicate skin.